Prof. Peter Gordon Watson (30 April
1930 – 31 January 2017) was a British ophthalmologist, professor, and
researcher.
Unlike Cairns’ so-called trabeculectomy
procedure (which was more like a canaloplasty) in which aqueous was assumed to
flow through the cut ends of the Schlemm’s canal, the Watson-Barnett
modification consisted of excision of a block of sclero-cornea and allowing
posterior filtration of aqueous through the sclerostomy (therefore, this
procedure can be called a “sclerokeratectomy”).
The procedure was performed on 90 eyes in
60 patients between 1967 and 1972.
The follow-up ranged from one to six years
postoperatively. (In 24 cases the follow-up was more than five years).
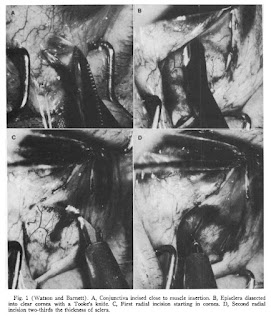
The procedure involved the creation of a wide
conjunctival flap. This was followed with two radial incisions backward from
the corneoscleral limbus, 4 to 5 mm long and 5 mm apart through two-thirds of
the scleral thickness. The ends of these incisions joined a third
circumferential incision in the sclera. This led to the formation of a scleral
flap hinged anteriorly just into the clear cornea.
The deep flap containing the scleral spur
and trabecular meshwork was now dissected. An incision through the remainder of
the sclera was made transversely behind the scleral spur. It was readily
identifiable by its fine white texture in contrast to the gray ciliary body
posteriorly and the clear trabecular tissue with underlying brown iris tissue
anteriorly.
Another pair of incisions were made passing
through the full thickness of the cornea and sclera, and extending backward
from the corneoscleral limbus posteriorly to the transverse incision.
The iris rarely bulged into the wound at
this stage, but if it did, a small iridotomy released the aqueous humor from
the posterior chamber and the iris fell back.
The superficial flap was replaced and
sutured to the sclera. The number of sutures required depended on how well the
incisions were apposed. If there was a retraction of the scleral edges,
multiple or continuous sutures of 8-0 virgin silk or 10-0 Perlon or Ethilon
were used. If the edges were well apposed, only three sutures of 8-0 virgin
silk were needed in the posterior flap.
The conjunctiva was closed with continuous
8-0 virgin silk suture.
COMPLICATIONS:
INTRAOPERATIVE= In four eyes it was difficult
to re-form the anterior chamber at the end of the procedure. One patient had prolonged
bleeding from a ciliary process at the time of the iridectomy, however
eventually it stopped spontaneously. The ciliary body prolapsed into the wound
in another eye when the transverse incision was made in the deep flap.
POSTOPERATIVE= Flat AC was seen in two eyes
on the first postoperative day and returned to normal later. Six eyes had
shallow AC in the immediate few days after surgery and five eyes developed
shallow AC later. Hyphemas large enough to form a fluid level were seen in 17
eyes (19%) postoperatively. Uveitis was seen in ten eyes. There was further
loss of the visual field in one eye despite an average intraocular pressure of
15 mm Hg. In 16 eyes (18%) visual acuity deteriorated after operation.
Progression of pre-existing cataract was seen in 14 eyes, corneal edema in one
patient, and no cause was found in one patient.
RESULTS:
In 87% of the eyes, IOP was controlled
without further medications or surgery. In 82 eyes (91%) a bleb formed, but in
8 (8.8%) the IOP was controlled with no evidence of bleb formation.
IOP
was controlled at the outset in 84% of the eyes and eventually controlled in
over 97%. Only 11% of the eyes required further medication and 5.5% further
surgery.











No comments:
Post a Comment