INTRODUCTION:
Patients with early glaucoma often complain of more severely compromised visual quality than would be expected despite their good documented visual acuity (VA). This discrepancy is most likely due to glaucomatous damage causing a decrease in the ability to perceive contrasting boundaries.
As compared with VA, contrast sensitivity is correlated better with target identification during driving, walking, and identification of images, such as faces.
Subtle loss of both central and peripheral vision can be demonstrated in some patients with glaucoma, before visual field changes are detectable with standard techniques. This can be done by measuring the amount of contrast required for a patient to discriminate between adjacent visual stimuli.
In some studies, the contrast sensitivity impairment correlates with visual field (in terms of Mean deviation=MD), especially with the central visual field and optic nerve head damage.
PATHOPHYSIOLOGY:
There is histologic evidence for a reduction in the proportion of larger retinal ganglion cells (RGCs) in glaucomatous eyes, both in human and in experimental primate models of glaucoma.
Although many types of RGC have been identified there are three major classes of RGCs that are currently well understood: namely, the parvocellular (P), magnocellular (M), and koniocellular (K) RGCs. These cell types can be distinguished both functionally and morphologically.
In terms of morphology, parvocellular RGCs are on average smaller than M or K neurons; hence, one possible inference from histologic studies of glaucomatous eyes is that people with glaucoma should show dysfunction on tasks mediated by M or K neurons but relative sparing of visual tasks dominated by P input.
Morgan et al. classified primate RGCs as parasol (presumed M) or midget (presumed P) and found that the ratio of parasol to midget cells was relatively preserved in glaucomatous eyes, although the total number of cells were reduced.
Studies suggest that both larger and smaller cell types shrink before death in glaucoma but that larger cells may be more susceptible to this process.
Yucel et al. have demonstrated approximately equivalent loss of the M and P layers of the lateral geniculate nucleus (LGN) in experimental primate glaucoma. However, Chaturvedi et al. found a greater loss of neurons from M layers in autopsied human LGN. Crawford et al. studied metabolic activity of neurons in the LGN of primates with experimental glaucoma and found similar reductions in cytochrome oxidase reactivity in P and M layers.
Studies have reported SPATIAL summation properties to differ between M- and P-mediated pathways. However, the underlying spatial summation properties associated with these pathways were similar in control patients and those with glaucoma.
In a study comparing the decrease in contrast sensitivity between normal aging and glaucoma, aging decreased low-spatial frequency sensitive components of both the M and P pathways. Glaucoma results in a further reduction of sensitivity that does not seem to be selective for M or P functions, which the investigators presumed were mediated by cells with larger receptive fields.
TEMPORAL contrast sensitivity, in which the patient must detect a visual stimulus flickering at various frequencies, provides another measure of contrast sensitivity and appears to be more useful than spatial contrast sensitivity in patients with glaucoma. The stimulus may be presented as a homogeneous flickering field (flicker fusion frequency) or as a counter-phase flickering grating of low spatial frequency (spatiotemporal contrast sensitivity). Patients with glaucoma may have reduced function with either method, although the latter appears to be a more sensitive test.
Visual function in glaucomatous eyes, as measured by contrast sensitivity, has been shown to improve after beta-blocker therapy.
CONTRAST SENSITIVITY TESTING IN GLAUCOMA:
The human contrast sensitivity can be quantified via 4 parameters namely, peak sensitivity, peak frequency, bandwidth, and low-spatial frequency truncation.
The yield of detecting glaucoma may be increased by measuring peripheral contrast sensitivity, 20 to 25 degrees eccentrically.
Many standard contrast sensitivity tests for clinical purpose use foveal viewing of paper charts [eg, Pelli Robson (PR) chart, Mars Letter Contrast Sensitivity Test, Vistech VCTS 6500 charts, Regan Low contrast letter acuity charts] and cards (eg, Hamilton-Veale Contrast Sensitivity). Cathode ray tube computerized testing is more precise and flexible.
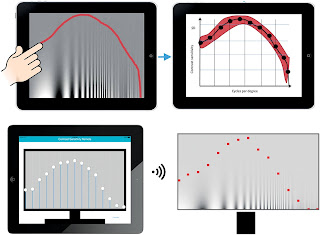
Mobile apps such as Aston contrast sensitivity test have also made contrast sensitivity assessment less time consuming. Although, there is a difference in sensitivity measures obtained via the apps and the PR chart.
The Spaeth Richman Contrast Sensitivity test (SPARCS) is an internet-based test that features multiple answer choices and a bracketing technique to determine contrast threshold. SPARCS measures contrast sensitivity in both central and peripheral quadrants giving it an additional parameter to assess glaucomatous damage as compared with the tests which measure only central contrast sensitivity.
Richman and colleagues have shown that a total SPARCS score of <70 has been shown to have 80% sensitivity and 93% specificity for glaucoma.
Patients with ocular hypertension and glaucoma demonstrate contrast sensitivity losses at spatial frequencies between 0.25 and 8 cpd.
Bambo et al., Hawkins et al. and Wilensky et al., reported a significant correlation between the mean deviation as measured with the Humphrey perimeter and the Pelli-Robson contrast sensitivity scores.
Clinical assessment of M pathway function (for example, FREQUENCY-DOUBLING PERIMETRY) has been popular not only because of the notion that larger RGCs may be lost first in glaucoma, but also because of the suggestion that assessment of pathways with reduced redundancy is more likely to manifest a deficit.
Some studies suggest that specific measures of P-pathway function may be equally as effective as assessing M function for the detection of early glaucoma. This finding is consistent with a number of previous studies that have identified visual deficits in people with early glaucoma using tasks that are understood to be processed predominantly by the parvocellular pathways.
Nawi et al. have evaluated acquired color vision deficiency in glaucoma by using the Rabin cone contrast test (RCCT). The chromatic discrimination thresholds measured by RCCT in the glaucoma group were significantly different from those measured in the control group and correlated with the MD and macular ganglion cell/inner plexiform layer (GCIPL) thickness.
CONCLUSION:
Contrast sensitivity is significantly decreased as the severity of glaucoma increases, and this could account for the common complaint of patients with glaucoma of hazy or blurry vision despite good VA. In a study, contrast sensitivity was more closely related than color perception or reading ability with disease severity.
FURTHER READING:
Shields Textbook of glaucoma. 6th edition.
Ichhpujani P, Thakur S, Spaeth GL. Contrast sensitivity and glaucoma. J Glaucoma 2020;29:71–75.
Bambo MP, Ferrandez B, Güerri N, et al. Evaluation of Contrast Sensitivity, Chromatic Vision, and Reading Ability in Patients with Primary Open Angle Glaucoma. J Ophthalmol. 2016;2016:7074016. doi:10.1155/2016/7074016.
McKendrick AM, Sampson GP, Walland MJ, Badcock DR. Contrast sensitivity changes due to glaucoma and normal aging: low-spatial-frequency losses in both magnocellular and parvocellular pathways. Invest Ophthalmol Vis Sci. 2007;48(5):2115-2122. doi:10.1167/iovs.06-1208.
Niwa Y, Muraki S, Naito F, Minamikawa T, Ohji M. Evaluation of acquired color vision deficiency in glaucoma using the rabin cone contrast test. Invest Ophthalmol Vis Sci. 2014;55:6686–6690. DOI:10.1167/iovs.14-14079.







No comments:
Post a Comment