PRIMARY CONGENITAL GLAUCOMA
Guest author
SABEEH
Ajmal Khan Tibbiya Colege
Aligarh, India
Introduction
Primary
Congenital Glaucoma (PCG) is a potentially blinding disease of children, which if
untreated, would result in a lifetime of blindness. It occurs due to
obstruction of the drainage of the aqueous humor caused by a primary developmental
anomaly at the angle of anterior chamber. Although PCG
is the most common glaucoma seen in infancy, it is still an uncommon disease.
The variable incidence in various ethnic groups points towards a genetic basis
for the disease.
Epidemiology
- The disease varies sustainability in different ethnic groups from 1:1250 births in Slovakian Roms to 1:20,000 in Scandinavian regions.
- In the West, the average incidence is about 1:10,000 births, but appears to be higher in Asians.
- In Saudi Arabia, it is reported to be 1:2500, while Indian's have incidence of 1:3300.
- The disease was responsible for 4.2% of blindness in the pediatric population.
Inheritance
- Most cases of PCG are sporadic in occurrence.
- Recessive inheritance of some cases of PCG is proved by:
- A high frequency of parental consanguinity.
- The presence of disease in about 25% of sibs of probands.
- The presence of the disease in all children of a marriage between 2 affected persons.
- The occurrence of Glaucoma in collaterals of both parents some families.
Genetic defects
- According to Human Genome Organization (HUGO) Nomenclature Committee, loci for congenital glaucoma are designated by GLC3 and letters are added to distinguish specific loci in order of their discovery.
- Till date, 3 genetic loci have been linked to PCG:
- GLC3A at chromosome locus 2p21.
- GLC3B at chromosome locus 1p36.
- GLC3C at chromosome locus 14g24.3
- Of these only the GLC3A locus has been linked to a specific gene. This gene is called CYP1B1 and is the largest known enzyme of the human cytochrome p450 pathway.
- There are several known missense mutations within the CYP1B1 gene.
- Among these, the mutations identified are:
- G61E, Ter223, P193L, E229K, R390C, R368H.
- A study on the genotype-phenotype correlation of these patients identified the frame shift mutation and R390C homozygous mutation as being associated with very severe disease and poor prognosis regardless of any treatment.
Structural defects and clinical
features
- The glaucomas are a heterogeneous group of insidious diseases associated with elevated IOP and optic nerve atrophy.
- Primary Congenital Glaucoma is a specific, inherited developmental defect in the trabecular meshwork and anterior chamber angle.
- The developmental anomalies of the anterior chamber angle prevent drainage of aqueous humor, thereby elevating IOP.
- Elevation of IOP in children younger than 3 years of age causes rapid enlargement of the globe, occurs primarily at the corneo-scleral junction.
- As the cornea and limbus enlarge, the endothelium of the cornea and Descemets membrane are stretched. This stretching can result in a linear rupture of Descemet's membrane known as Haab's striae.
- The Descemet's membrane ruptures may occur acutely causing an influx of aqueous into the stroma and epithelium resulting in sudden corneal edema.
 |
| Haab's striae |
Clinical
features of PCG typically include:
- Tearing
- Photophobia
- Buphthalmos (enlargement of the globe)
- Clouding of the cornea
More
serious consequence of elevated IOP is that it can rapidly lead to axonal loss
and permanent visual impairment in untreated children.
 |
| Buphthalmos |
Management
The
management of Congenital Glaucoma starts with parental counseling, which
includes discussion for: need for surgery and possibilities of multiple
surgeries; the need for lifelong follow up and the combination of problems to
be tackled (IOP, amblyopia management, refractive correction, possible
keratoplasty).
Panicker
and associates have graded the severity of glaucoma depending upon the clinical
features as given below in table.
SEVERITY
INDEX FOR GRADING PCG
|
Clinical parameters
used for grading
|
Normal
|
Mild
|
Moderate
|
Severe/Very severe
|
|
Corneal
diameter
|
Upto
10.5mm
|
>10.5-12mm
|
>12-13mm
|
>13mm
|
|
IOP
|
Upto
16 mmHg
|
>16-20
mmHg
|
>2030
mmHg
|
>30mmHg
|
|
C/D
ratio
|
0.3-0.4
|
>0.4-0.6
|
>0.6-0.8
|
>0.8
|
|
Last
recorded VA
|
20/20
|
|
|
<20/400-NPL
|
|
Corneal
opacity
|
No
edema
|
Mild
edema
|
Severe
edema
|
Severe
edema+Haab’s striae
|
Examination under anesthesia is an essential part of PCG management. It includes the following examinations:
 |
| EUA |
Tonometry
General
anesthesia usually lowers the IOP, except for ketamine.
The
Tono-pen is convenient and easy to use.
The
normal IOP in infants under anesthesia is usually in the low teens.
A
pressure of 20 mmHg or more should be considered abnormal.
Corneal
diameter
Using
calipers the corneal diameter measurement should be taken from limbus to a
similar point 180-degree away at the opposite limbus.
The
95% ranges of normal corneal diameters are: 9.4 mm to 11 mm at age 1 month,
10.5 mm to 11.7 mm at age 6 months, and 10.8 mm to 12 mm at age 12 months.
In
PCG, the diameter of cornea may enlarge to as much as 17 mm.
Changes
in the corneal diameter less than 0.5 mm in the follow up examination should be
interpreted cautiously.
Gonioscopy
A
14 mm Koeppe lens provides a clear view of the angle of the eye and a hand held
microscope with a Barkan light or any type of illuminator is necessary for
gonioscopy during anesthesia.
In
Congenital Glaucoma the Iris usually is inserted anterior to scleral spur and
the angle recess is poorly formed.
Fundoscopy
Dilated
fundus examination and disc evaluation are essential in diagnosing congenital
glaucoma.
Optic
nerve cupping larger than 30% of the disc diameter, especially if asymmetric
between two eyes, is strong evidence that the disc is under pressure and may be
glaucomatous.
Glaucomatous
cupping in infants, unlike adults is usually reversible after normalization of
IOP.
The
younger the child, the faster is the reversibility.
Surgical treatment
The
surgical options include:
Goniotomy
Trabeculectomy
Trabeculectomy
with anti-fibrotic agents
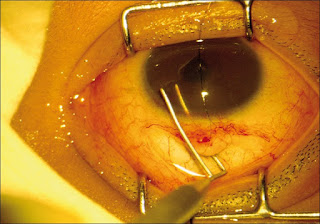
 |
| Goniotomy |
A
trabeculotomy-trabeculectomy combined surgery has been found to result in more
favorable outcomes and many surgeons prefer that approach.
In
case of refractory cases not responding to surgery, a repeat surgery is needed.



No comments:
Post a Comment