PLATEAU IRIS
Guest Author
SHIBRA FAROOQ
Ajmal Khan Tibbiya College
Aligarh, India
INTRODUCTION
Plateau
iris is a type of narrow angle more commonly seen in younger adults that can
lead to chronic angle closure glaucoma. Plateau iris is caused by a narrowing
of the anterior chamber angle due to insertion of the iris anteriorly on the
ciliary body or displacement of the ciliary body anteriorly, which in turn
alters the position of the peripheral iris in relation to the trabecular
meshwork (i.e. placing them in apposition).
Plateau
iris syndrome is defined as a persistently narrow angle capable of closure despite
a patent iridotomy.
Plateau
iris is an ocular condition that requires appropriate diagnosis and treatment
in order to prevent vision loss.
DISEASE
ENTITY
The
term plateau iris was first used in 1958 to describe a unique configuration of
the iris.
In
1977, a study of 8 patients who presented with angle closure glaucoma after an
iridotomy helped clarify the condition.
In
order to avoid confusion, the term plateau iris configuration (PIC) and plateau
iris syndrome (PIS) were distinguished.
PIC
is a pre-operative condition in which appositional or narrow angle is confirmed
by gonioscopy; however, the anterior chamber depth is normal and the iris is
flat. In PIC, the iris root angulates forward peripherally and then centrally
in a planar fashion.
PIS,
on the other hand, is a post-operative condition in which a patent iridotomy
has eliminated the relative pupillary block that is normally seen in an
appositional angle or primary angle closure glaucoma, but evidence of
angle-closure persists without shallowing of the anterior chamber. PIS most
commonly occurs in the early postoperative period, however, it can also occur
years after surgery.
ETIOLOGY
PIC
is characterized by an appositional angle with a flat iris configuration, in
contrast to an anterior bowing of the iris seen in a “typical angle closure
glaucoma” in which there is a more crowded anterior chamber due to a hyperopic
eye (short axial length). In patients with PIC, the iris root is often short
and inserted anteriorly on the ciliary face, causing a shallow and narrow
angle. With plateau iris configuration, there is a relative pupillary block
mechanism.
Plateau
iris syndrome is due to an abnormal anterior position of ciliary body. This
anterior ciliary body displacement in turn alters the position of the peripheral
iris in relation to the trabecular meshwork resulting in obstruction to aqueous
outflow. Therefore, the etiology of plateau iris syndrome is distinct from that
of most cases of angle closure glaucoma, which is usually caused by a relative
pupillary block. PIS may be triggered by spontaneous pupillary dilatation (for
e.g. in conditions of darkness) or in response to mydriatic agents.
EPIDEMIOLOGY
Plateau
iris syndrome is well recognized as a common etiology of angle closure in
relatively young patients.
The
prevalence of PIS was found to be approximately 32% by UBM after laser
peripheral iridotomy (LPI) in a Singapore study in eyes at risk for primary
angle closure in individuals greater than 50 years.
In
another review, the prevalence of PIS was 64% in individuals less than 60 years
old with recurrent symptoms of angle closure despite a peripheral iridotomy or
iridectomy.
Patients
with PIS tend to be young, female and less hyperopic than those with angle
closure glaucoma caused by relative pupillary block.
In
a large retrospective analysis by Ritch et al, the mean age of diagnosis for
patients with PIS was 35.
Other
potential causes of angle closure in young patients include iridociliary cysts,
lens-induced angle closure, nanophthalmos, retinopathy of prematurity, uveitis
(posterior synechiae), lens subluxation and a variety of other rare clinical
conditions.
PATHOPHYSIOLOGY
If
the flow is impeded in any way, IOP will rise. In a patient with plateau iris
configuration, the iris root is short and the ciliary body processes may be
larger and more anteriorly positioned than normal. This results in a mechanical
repositioning of the peripheral iris (i.e. “bunching” or focal aggregation of
the peripheral iris), thereby crowding the angle and obstructing flow through
the trabecular meshwork.
In
either case, this anatomic abnormality obstructs the flow of aqueous fluid
through the trabecular meshwork causing an increase in IOP and angle-closure
glaucoma.
PRIMARY
PREVENTION
Plateau
iris -configuration/-syndrome are anatomical abnormalities that should be kept
in the differential diagnosis of patients with narrow angles or appositional
angle closure, as the condition has potential to cause permanent vision loss.
This condition occurs in a relatively young patient population so screening for
plateau iris in young patients with symptoms of angle closure should not be
delayed.
DIAGNOSIS
HISTORY
The
diagnosis of plateau iris is most commonly made in asymptomatic patients on
routine examination of the eye.
Patients
with plateau iris tend to be female, in their 30-50s, hyperopic and often have
a family history of angle-closure glaucoma.
Symptomatic
patients present with headaches, eye pain, nausea and vomiting: symptoms that
are indicative of an acute rise in IOP.
The
patient may also complain of seeing halos around lights or blurring of vision.
Symptoms are more likely to occur after dilatation of the pupil.
PHYSICAL
EXAMINATION
Slit-lamp
examination of patients with plateau iris configuration usually shows a normal
anterior chamber depth and a flat iris plane.
A
“double-hump sign” on indentation gonioscopy is characteristically seen in this
condition. The peripheral “hump” on the iris is caused by the ciliary body
propping up the iris root, whereas the central “hump” represents the central
third of the iris resting over the surface of the lens.
 |
| "Double-hump sign" |
Ultrasound
biomicroscopy (UBM) plays a fundamental role in the diagnosis of PIC/PIS, as
this modality can definitely confirm the anatomic abnormalities of the ciliary
body. In patients with PIC or PIS, UBM will show anteriorly situated ciliary
processes and in some cases a shortened, thickened iris root that is inserted
in a more anterior position in the ciliary body.
DIFFERENTIAL
DIAGNOSIS
Other
possible diagnoses include:
- Pupillary block (relative or absolute)
- Iridociliary cysts (“Pseudoplateau iris”)
- Peripheral anterior synechiae
- Lens-induced angle closure (“Phacomorphic glaucoma”)
- Nanophthalmos
MANAGEMENT
MEDICAL
THERAPY
The
primary treatment modality for many patients with plateau iris configuration is
surgical.
Many
clinicians, however, will first treat with miotic agents such as pilocarpine to
prevent pupillary dilatation leading upto surgery. Low dose or dilute pilocarpine
can produce thinning of iris and facilitate opening of the angle by pulling the
iris away from the trabecular meshwork.
SURGERY
Since
patients with PIC often have an element of pupillary block, peripheral laser
iridotomy is the first surgical intervention performed. A peripheral iridotomy,
however, does not change the anatomy of the anterior chamber, so some patients
with PIC may still experience a glaucoma crisis (the patient should now be
considered PIS, not PIC).
If
a peripheral iridotomy is unsuccessful in controlling the IOP (i.e. confirmed
PIS), the treatment of choice is argon-laser peripheral iridoplasty (ALPI).
This procedure is highly effective in eliminating appositional residual closure
caused by PIS.
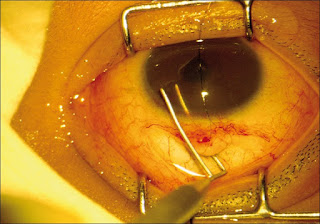
 |
| PI & ALPI in same eye |
If
peripheral iridotomy, ALPI and additional miotic agents fail to adequately
control IOP, then surgical procedures such as trabeculectomy, drainage
implantation or goniosynechiolysis should be considered.
PROGNOSIS
The
prognosis for patients with PIC/PIS is generally good, provided the condition
is recognized before vision loss occurs.
Regular
follow-up with serial gonioscopy ensures that the proper interventions and
treatment modalities are initiated when necessary because angle-closure may
develop years after successful iridotomy or iridoplasty.
Routine
screening for the development of glaucoma should also be performed.