Endoscopic cyclophotocoagulation (ECP)
is a procedure to lower aqueous production by laser-induced destruction of the
ciliary processes, the site of aqueous production in the eyes. The key feature
of ECP is direct visualization of the ciliary processes as the target tissue
for controlled laser ablation. With this procedure, it is possible to titrate
the extent of ciliary body ablation to maximize IOP lowering while minimizing
collateral damage and adverse events. It can be performed along with cataract
surgery or as a stand-alone treatment.
The ECP instrumentation consists of the
laser endoscope and the console to which it is attached. The laser endoscopy
console combines a 175 W xenon light source for illumination, 810 nm diode
laser for photocoagulation, helium-neon laser aiming beam, and video imaging
for intraocular visualization.
The endoscopy probe contains all three
fiber groupings and is available in 19, 20, or 23 gauge sizes with a field of
view ranging from 70° to 140° and depth of focus spanning 1–30 mm. The probe
tips are straight or curved and easily fit through a 2.0 mm clear corneal
incision. Another advantage to the 23-gauge probe is its compatibility with all
23-gauge vitrectomy trocar systems. The probes can be sterilized and reusable
up to 25 times or more.
A variety of anesthesia may be used for
ECP including intracameral, sub-Tenon's, or retrobulbar routes of
administration. If intracameral anesthesia is utilized, increased intravenous
sedation may be needed to maximize patient comfort during the laser application.
Before the start of the procedure, the
three component cables of the ECP probe should be securely connected to the
laser console. The camera image should be focused with the desired orientation
and illumination adjusted outside the eye before the initiation of surgery. The
laser should be set to continuous duration with an initial power of 0.25 W and
an aiming beam setting of 20–30.
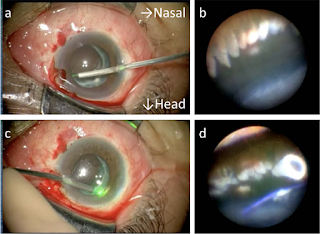
A temporal or superiorly placed clear
corneal incision is performed near the limbus, approximately 2.0 mm in width.
The ciliary sulcus is deepened with cohesive viscoelastic to improve
visualization of the ciliary processes. The probe is then inserted through the
corneal wound and positioned in the sulcus at or near the pupillary border.
The surgeon then directs his/her gaze
towards the monitor to gain orientation in the sulcus and identify the target
tissue. During treatment, approximately 6-7 ciliary processes should be in view
at all times as this places the probe at an optimal distance for absorption of
laser energy. Once the aiming beam is placed over a ciliary process, the foot
pedal is depressed to deliver laser energy continuously. Treatment is titrated
according to the visualized tissue response. The process should whiten and
shrink to a variable degree after appropriate treatment.
If the probe is closer to the
processes, a shorter duration and/or lower power will be needed to reach the
desired effect. Rupture or popping of the processes should be avoided as an
indication of over-treatment. The probe can then be advanced along the adjacent
processes while applying laser energy. The entire visible area of each ciliary
process should be treated including anterior and posterior edges as well as
crypts in between processes.
Treatment should be carried to the
extent of visualization in one direction, and then the probe is rotated 180°
with rotation of the image on the monitor, and treatment is continued as far as
possible in the other direction. With a curved probe, a single incision allows
treatment of approximately 270° of ciliary processes. If more treatment is
desired, a second incision may be placed 180° away from the initial wound to
gain access to the subincisional processes and complete a 360° treatment for
additional IOP lowering.
In aphakic or pseudophakic patients, a
pars plana approach (ECP plus) may also be utilized to achieve a more thorough
treatment of the ciliary processes when aggressive IOP lowering is desired. A
standard 2 or 3 port pars plana vitrectomy must be performed initially,
followed by insertion of the probe through one of the sclerotomies. Once the
processes are visualized, treatment is carried out in the same fashion as the
anterior approach. The anterior 1-2 mm of pars plana may also be treated in
severe, refractory cases but may increase the risk for hypotony
postoperatively.
At the end of the procedure
viscoelastic is removed and the incision/s coapted.
Postoperatively the patient is started
on steroid drops until the inflammation resolves. The anti-glaucoma medications
are continued until the inflammation subsides and the desired IOP is achieved.
REFERENCE:
Seibold LK, SooHoo JR, Kahook MY.
Endoscopic cyclophotocoagulation. Middle East Afr J Ophthalmol. 2015
Jan-Mar;22(1):18-24. doi: 10.4103/0974-9233.148344. PMID: 25624669; PMCID:
PMC4302471.











No comments:
Post a Comment