DR. SHIBRA FAROOQ
P.G. SCHOLAR
DEPARTMENT OF ILAJ-BIT-TADBEER
AJMAL KHAN TIBBIYA COLLEGE,
ALIGARH MUSLIM UNIVERSITY, INDIA
This post discusses two meta-analyses that
analyze the association of hypertension with glaucoma.
META-ANALYSIS 1:
Bae HW, Lee N, Lee HS, Hong S, Seong GJ,
Kim CY. Systemic hypertension as a risk factor for open-angle glaucoma: a
meta-analysis of population-based studies. PLoS One. 2014 Sep 25;9(9):e108226.
doi: 10.1371/journal.pone.0108226. PMID: 25254373; PMCID: PMC4177901.
The association between hypertension and
glaucoma is controversial. It is usually assumed that hypertension increases
the risk of development and progression of glaucoma.
In the Blue Mountains Eye Study,
hypertension increased the risk of open-angle glaucoma (OAG) by more than 50%. The
Egna-Neumarkt Study also found an association between OAG and hypertension. However,
the Barbados Eye Study did not find an association between the two.
Hypertension can cause damage to the optic
nerve through multiple mechanisms. These include direct microvascular damage,
impairing the blood flow to the anterior optic nerve; auto-regulation of the
posterior ciliary circulation; and induction of hypotensive episodes,
especially at night, by anti-hypertensive therapy, which can injure the optic
nerve.
A meta-analysis to look into systemic
hypertension as a risk factor for OAG was performed by Bae et al. The
meta-analysis included 16 studies involving 60,084 individuals.
The present meta-analysis of
population-based studies showed that individuals with hypertension have an
approximately 1.2-fold higher risk of developing OAG than individuals without hypertension.
The pooled odds ratio (OR) was 1.22 (95% CI: 1.09–1.36) using the fixed-effects
model and 1.22 (95% CI: 1.08–1.37) using the random-effects model.
The study found that hypertension increased
the risk of OAG development irrespective of age.
The risk of developing high-tension
glaucoma (HTG) was increased to a greater extent by hypertension than that of
OAG, whereas the risk of developing normal-tension glaucoma (NTG) was not
affected by hypertension (OR=1.92 and 0.94, respectively). This difference
might be attributable to the difference in IOP, which is related to ocular
perfusion pressure (OPP).
There are two conflicting mechanisms
involving hypertension and glaucoma. Increased BP leads to reduced ocular blood
flow due to thickening and stiffening of the vessel wall, thereby increasing
the risk of OAG. The second mechanism is that a higher BP produces a higher
OPP, which could decrease the risk of OAG.
No significant regional differences between
Eastern and Western populations were noted.
META-ANALYSIS
2:
Nislawati R, Taufik Fadillah
Zainal A, Ismail A, et al. Role of hypertension as a risk factor
for open- angle glaucoma: a systematic review and meta-analysis. BMJ Open
Ophthalmology 2021;6:e000798. doi:10.1136/ bmjophth-2021-000798.
The relationship between blood pressure
(BP) and the incidence of glaucoma is still being debated.
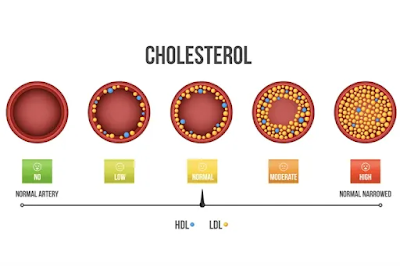
Several studies have reported that BP and
intraocular pressure (IOP) are directly related. This is because elevated BP
increases episcleral venous pressure so that the aqueous outflow decreases,
leading to an increase in IOP.
However, in younger patients, systemic
hypertension (HTN) has a protective effect by increasing the ocular perfusion
pressure (OPP).
A meta-analysis by Nislawati et al has
shown that individuals with systemic HTN had a significantly 1.71- fold risk of
developing glaucoma compared with non-hypertensive people (1.71 (95% CI 1.58 to
1.85)).
It is reported that a 10 mm Hg increase in
systolic BP resulted in an increase in IOP by 0.26 mm Hg, whereas an increase
in diastolic BP by 5 mm Hg increased IOP by 0.17 mm Hg.
The average age of patients with open-angle
glaucoma (OAG) was higher with a mean difference result (4.21 (95% CI 0.7 to
7.72)). The results of another meta-analysis showed that the female gender had
a higher risk of experiencing OAG with the result of a risk ratio (1.3 (95% CI
1.2 to 1.41)). This shows that HTN, age, and gender also contribute to the
incidence of OAG.
High BP can increase IOP through two
mechanisms, first, an increase in the production of aqueous humor, which is
caused by an increase in capillary pressure in the ciliary body, thereby
increasing the intravascular pressure and IOP gradient; second, decreasing the
absorption of aqueous humor by increasing the episcleral venous pressure which
obstructs the outflow of aqueous humor from the eye.
In hypertensive patients, glaucoma damage can
also occur due to decreased perfusion pressure causing ischemia of the optic
nerve or retinal ganglion cells (RGCs). HTN causes a narrowing of the caliber
of the central retinal artery (CRA), which results in impaired flow to the eye,
especially in the ocular nerve head and lamina cribrosa.
Unlike the positive effect of hypertension
in younger patients, chronic elevated BP in the elderly increases the risk of
arteriosclerosis, changes in precapillary arteriolar size leading to increased
resistance to blood flow and resulting in decreased perfusion in the posterior
segment of the eye, thereby counteracting the protective effect prevailing at
younger ages.
Hypertension can cause autoregulation
disorders resulting from an imbalance in endothelin-1 levels.
The analysis found that decreased Diastolic
BP (DBP) can reduce perfusion pressure in the eye, which increases the risk of
OAG. These studies show that individuals with unstable DBP, either high DBP or
low DBP, are at increased risk of OAG.
CONCLUSION:
These meta-analyses which analyzed studies
involving thousands of patients worldwide, have found a positive association
between hypertension and glaucoma. Therefore, patients with hypertension should
be assessed for glaucoma more diligently.