TONOMETERS
INTRAOCULAR PRESSURE (IOP):
Normal IOP may be defined as that pressure which does not
lead to glaucomatous optic nerve head damage. IOP is determined by a balance
between production and drainage of aqueous humor in the eye. Normally, the IOP
ranges from 10-21 mmHg.
FACTORS EXERTING LONG-TERM INFLUENCE
ON IOP
|
FACTORS EXERTING SHORT-TERM INFLUENCE
ON IOP
|
1.Genetics
|
1. Diurnal variation
|
2.Age
|
2. Postural variation
|
3.Sex
|
3. Exertional influences
|
4.Refractive error
|
4.Lid and eye movement
|
5.Race
|
5. Intraocular conditions
|
6. Systemic conditions
|
|
7. Environmental conditions
|
|
8. General anesthesia
|
|
9. Food and drugs
|
TONOMETERS:
Tonometers are used to measure
IOP. They are of different types depending on the shape of deformation they
produce.
INDENTATION TONOMETERS:
In indentation tonometry the shape of deformation is in the form of a truncated cone. However, the precise shape is variable and unpredictable. The tonometer also displaces a relatively large intraocular volume. As a result of these peculiar characteristics, conversion tables have been developed to calculate IOP. These tonometers are also affected by scleral rigidity. Thin scleras giving abnormally low and thick/rigid scleras giving abnormally high IOP values. An example is the Schiotz tonometer.
INDENTATION TONOMETERS:
In indentation tonometry the shape of deformation is in the form of a truncated cone. However, the precise shape is variable and unpredictable. The tonometer also displaces a relatively large intraocular volume. As a result of these peculiar characteristics, conversion tables have been developed to calculate IOP. These tonometers are also affected by scleral rigidity. Thin scleras giving abnormally low and thick/rigid scleras giving abnormally high IOP values. An example is the Schiotz tonometer.
 |
| Schiotz tonometer |
APPLANATION
TONOMETERS:
In applanation tonometers the
shape of deformation is simple flattening. Since the shape is constant, its
relationship to IOP can be derived from mathematical calculations. Applanation
tonometers are of 2 types: (1) Variable force: It measures the force
required to applanate (flatten) a standard area of the corneal surface e.g.
Goldmann Tonometer (GT). (2) Variable area: It measures the area of the
cornea, which is flattened by a known force (weight), e.g. Maklakov Tonometer.
 |
| Goldmann Applanation Tonometer |
The GT is regarded as a gold
standard in IOP evaluation. Goldmann based his tonometer on the Imbert-Fick
law, a modification of the Maklakov-Fick law. According to this law, the
external force (W) against a sphere equals the pressure in the sphere (Pt)
times the area flattened (applanated) by the external force (A).
W=Pt x A
However, the Imbert-Fick Law
has been modified to account for the surface tension, the force to bend the
cornea and inner area of flattening.
The cornea is anesthetized and
fluorescein is instilled. The tonometer head is slowly made to touch the
central cornea until the mires (semicircles) are visible. Subsequently, the
counter attached to the tonometer is turned till the inner parts of the mires
are in contact with each other.
Sources of error in
Goldmann tonometry:
1. Semicircles: Wider menisci cause falsely higher
pressure estimates. Improper vertical alignment will also lead to a falsely
high IOP estimate.
2. Corneal variables:
a. Thickness:
GAT works best at a central corneal thickness (CCT) of 525 µm. Thinner corneas
are associated with falsely low IOPs and thicker with falsely high IOP.
b. Curvature:
Increased curvature associated with falsely high IOPs. An increase of 1 mmHg is
seen with every 3Ds increase in corneal power.
c. Astigmatism:
IOP is underestimated for with-the-rule and overestimated for against-the-rule
astigmatism. There is 1 mmHg of error for every 4D of astigmatism. To minimize this
error rotate the biprism until the dividing line between the prisms is 450
to the major axis of the ellipse or an average of horizontal and vertical
readings taken. An irregular cornea also distorts the mires.
3. Prolonged contact: Leads to corneal injury as well
as a false lowering of IOP.
4. Calibration: Monthly calibrations of the
instrument are important to avoid errors.
Disinfection:
It is done by soaking the applanation tip for 5-15 minutes in diluted sodium
hypochlorite (1:10 household bleach), 3% hydrogen peroxide or 70% isopropyl
alcohol. The tip can also be wiped with alcohol, hydrogen peroxide,
povidone-iodine, 1:1000 merthiolate or dry tissues. Ten minutes of continuous
rinsing in running tap water removes HBV surface antigen.
REBOUND TONOMETER:
 |
| iCare |
An example of the rebound tonometer is the iCare device
(Helsinki, Finland). The iCare Pro can assess IOP with the patient lying down.
A 1.8 mm diameter plastic ball on a stainless steel wire is held in place by an
electromagnetic field in a handheld battery-powered device. When a button is
pushed, a spring drives the wire and ball forward rapidly. When the ball hits
the cornea, the ball and wire decelerate; the deceleration is more rapid if the
IOP is high and slower if the IOP is low. The speed of deceleration is measured
and is converted by the device into IOP.
No anesthetic is necessary for this device. It shows good
agreement with Goldmann and Tono-pen readings. However, IOP measurements
obtained with this tonometer are influenced by CCT, with higher IOP readings
with thicker corneas. This tonometer is also affected by other biomechanical
properties of the cornea, including corneal hysteresis (CH) and corneal
resistance factor (CRF). The disposable tips also increase the cost of the
instrument. An advantage is the small size, so it can be used in children and
those patients who have corneal abnormalities, including after corneal -grafts
or –implants (Corneal inlays or rings).
PASCAL DYNAMIC CONTOUR TONOMETER:
 |
| Pascal tonometer |
Dynamic contour tonometer (DCT) or Pascal tonometer (SMT
Swiss Microtechnology AG, Port, Switzerland) has a 7-mm diameter
concave-surface probe which adapts to the cornea’s contour and without altering
its shape or curvature. An electronic pressure sensor embedded in the
tonometer’s concave probe surface enables direct measurement of transcorneal
pressure. Nearly 100 IOP readings are taken per second. In contrast to the
Goldmann tonometer, measurements with the DCT are reported to be influenced less
by corneal thickness, and perhaps corneal curvature and rigidity. Some
measurement differences have been noted with the Goldmann Tonometer (mean
overestimation 2.3 mmHg). Therefore, the two tonometers may not be
interchangeably used. However, the DCT can provide valuable information in
persons whose corneal thickness is far from the mean or in patients who have
undergone refractive surgery. DCT can also be used to measure the ocular pulse
amplitude. The ocular pulse amplitude is defined as the difference between
diastolic and systolic intraocular pressure. The ocular pulse is generated by
the pulsatile ocular blood flow in the choroid. This forms a part of the
concept of vascular theory of glaucoma.
The instrument has to be used in conjunction with a slit-lamp,
has disposable tips which increase cost, requires prolonged tip contact and
specialized training to use it.
ORA AND CORVIS TONOMETERS:
ORA and CORVIS tonometers not only measure the IOP, but also
provide information on the biomechanical properties of the cornea and thus have
the potential to correct IOP readings for these factors. Corneal biomechanical
variables and the dynamic corneal behaviour can also be assessed independently.
Studies have shown that low corneal hysteresis is more likely a risk factor for
glaucoma, rather than CCT. Goldmann Tonometry is influenced by CCT, which
affects reliability of the instrument.
 |
| Ocular Response Analyzer |
Ocular Response Analyzer [ORA] (Reichert Inc., Depew, New
York, USA) is an airpulse tonometer. It utilizes a dynamic bi-directional applanation process to measure biomechanical properties of the cornea and IOP. A precisely collimated air-pulse causes the cornea to move inwards, past applanation, and into a slight concavity. Milliseconds after applanation, as the air pulse force decreases, the cornea begins to return to its normal configuration. In the process, it once again passes through an applanated state. An electro-optical system monitors the curature of the cornea throughout the deformation process, taking 400 data samples during the 20-millisecond measurement. 2 independent pressure values are derived from the inward and outward applanation events. A difference between the 2 gives the corneal hysteresis.
Thus, the ORA introduces two new concepts relating to the deformability of the cornea: corneal hysteresis (CH) and corneal response factor (CRF). These reflect the viscoelastic properties of the cornea. CH reflects the capacity of the cornea to absorb and dissipate energy and forms the basis for the instrument’s correction of IOP. The result of this correction is known as “corneal compensated IOP” (IOPcc). This new pressure is apparently less affected by corneal properties than that provided by a conventional applanation tonometer. The CRF indicates the overall resistance exerted by the cornea and is related to central corneal thickness and IOP. Whilst there is promising published evidence, the role of CH and CRF in the diagnosis and management of patients with glaucoma is yet to be fully established. The disadvantages are: The machine is fixed to a table and requires frequent maintenance. However, it does provide reliable IOP measurements.
Thus, the ORA introduces two new concepts relating to the deformability of the cornea: corneal hysteresis (CH) and corneal response factor (CRF). These reflect the viscoelastic properties of the cornea. CH reflects the capacity of the cornea to absorb and dissipate energy and forms the basis for the instrument’s correction of IOP. The result of this correction is known as “corneal compensated IOP” (IOPcc). This new pressure is apparently less affected by corneal properties than that provided by a conventional applanation tonometer. The CRF indicates the overall resistance exerted by the cornea and is related to central corneal thickness and IOP. Whilst there is promising published evidence, the role of CH and CRF in the diagnosis and management of patients with glaucoma is yet to be fully established. The disadvantages are: The machine is fixed to a table and requires frequent maintenance. However, it does provide reliable IOP measurements.
 |
| Corvis ST |
The Corneal Visualization Scheimpflug Technology Tonometer
[Corvis ST] (Oculus, Wetzlar, Germany) allows quantitative and visual assessment
of the biochemical properties of the cornea. The instrument incorporates an air
pulse tonometer and in-built pachymeter. The instrument incorporates an
ultra high-speed Scheimpflug camera and records the anterior chamber at the
moment of corneal deformation in real time. It measures variables related to
corneal deformability such as the time, velocity and length of the first and
second applanations, maximal concavity, and the deformation amplitude.
These biomechanical variables have to be assessed further to understand their
role in the development and progression of glaucoma.
TONO-PEN:
 |
| Tonopen |
The tonopen XL is based on the Mackay-Marg indentation
tonometer. It is a handheld instrument with a strain gauge that creates an
electrical signal as the footplate flattens the cornea(microstrain gauge
technology). It is portable, simple to use, can be used in both sitting and
lying positions and also offers easy calibration and use, by providing a
digital readout. The final IOP is calculated on the basis of 4 readings,
providing the coefficient of variation, which must be less than 5% for accurate
measurements. It has disposable latex covers; it can be used through contact
lenses and can be used over irregular corneas due to the smaller diameter of
the contact area (2.36 mm2 for tonopen, versus 7.35 mm2
for the GAT). While some studies found it to correspond to GAT measurements,
others found it to unreliable over IOPs above 20mmHg.
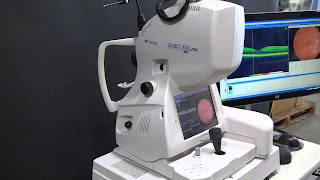
NON-CONTACT TONOMETER (NCT):
 |
| Non Contact Tonometer |
In this instrument a puff of room air is used to create a
constant force which deforms the central cornea. A collimated light beam
emerges from the machine and is detected by an optoelectronic system. The
moment the central cornea is flattened, the greatest numbers of light rays are
received by the detector, giving rise to the peak intensity of light. The point
from an internal reference point to the point of maximum light detection is then
converted into IOP.
The time interval for an average NCT to measure is 1-3
milliseconds (1/500th of a cardiac cycle). It is random to the phase of cardiac
cycle. Thus the ocular pulse becomes a significant factor in the detection of
IOP. In order to obviate that, 3 readings can be taken and an average
calculated.
SENSIMED TRIGGERFISH:
 |
| Sensimed Triggerfish |
The SENSIMED Triggerfish® (CLS, Sensimed AG, Lausanne,
Switzerland) consists of a silicone contact lens with an embedded pressure
sensor that enables continuous IOP monitoring. The sensor takes pressure
measurements over 30 seconds every 5 minutes to provide 288 measurements after
24 h of lens wear. The soft disposable contact lens embedded with a
miniaturised telemetric sensor detects the circumferential changes in the area
of the corneo-scleral junction. The IOP is calculated from the changes in ocular volume detected by the instrument. A flexible adhesive antenna worn around the eye
wirelessly receives from the contact lens the continuous acquired information
and transmits it to a portable recorder via a thin, flexible cable. The
portable recorder, worn by the patient, stores the acquired data during the
monitoring session. At the end of the recording period, the data is transferred
via Bluetooth from the recorder to the software previously installed on the
practitioner’s computer.
The software enables specialists to manage and visualise the
patient’s continuous IOP profile. The data provided by the SENSIMED
Triggerfish® complements punctual tonometer measurements and offers a
qualitative profiling of the patient’s IOP for up to 24 hours.
THE DIATON TONOMETER:
 |
| Diaton transpalpebral tonometer |
The Diaton tonometer is a hand
held device that measures IOP through the eyelid. It is useful to assess IOP
in the presence of ocular infections (keratitis), in patients after corneal
surgeries, with contact lenses on, in immobilized patients, to monitor IOP by
family members at home. Comparison with Goldmann applanation Tonometry was
found to give good results.