OPTICAL COHERENCE TOMOGRAPHY- ANGIOGRAPHY (OCT-A)
The vascular theory of glaucoma
attributes the development of glaucomatous changes to, among others, reduced
perfusion pressure, faulty vascular autoregulation and loss of neurovascular
coupling in the eye. However, the exact role of these factors is yet to be
elucidated. To some extent, this can be blamed on the lack of clinically
applicable imaging techniques to study vascular changes in glaucoma.
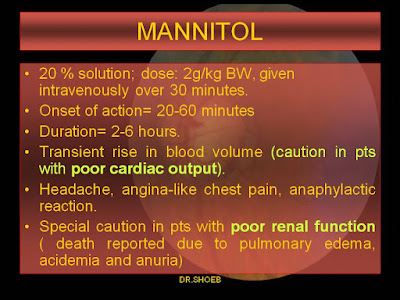
Conventionally, assessment of
retinal and choroidal circulations is done by Fluorescein Angiography (FA) and
Indo-Cyanine Green Angiography (ICG-A). However, these investigations require
intravenous administration of contrast agents which have certain limitations
such as contraindication of use in pregnancy and in patients with poor renal
clearance. The dye can also cause allergic reactions which can prove
life-threatening in susceptible individuals. These tests are hampered by their
ability to only provide 2-dimensional images with limited information regarding
the depth of the lesions.
Certain other non-invasive
imaging techniques have been utilized to visualize and quantify ocular
circulations. These include: Ultrasound Color Doppler, Functional Magnetic Resonance Imaging, Laser Doppler flowmetry and velocimetry, blue field entoptic technique
and laser speckle assessment. However, their clinical use is limited by their
complexity, poor reproducibility and wide variation in populations. Similarly, Doppler
OCT can also measure and quantify different blood velocities in larger vessels
but it is not well suited for retinal and choroidal microvasculature where
vessels are nearly perpendicular to the OCT beam.
OCT is a non-invasive, real-time
imaging modality, in common use all over the world. Over the last couple of
years, the advent of better and faster OCT machines has enabled the use of OCT-A
to obtain high resolution 3D angiograms of the retinal and choroidal vascular
networks. This allows detection of microvascular changes in glaucomatous eyes.

OCT-A detects the motion of red
blood cells (RBCs) using intrinsic signals to capture the location of blood
vessels. Thus, OCT-A identifies blood vessels by detecting the blood
flow-induced change in the OCT reflectance signal. The procedure requires
repeated B-scans at the same location to detect motion of the blood. This can
only be achieved by fast spectral-domain OCTs. RBCs flowing in the blood
vessels produce changes in the OCT reflectance signal, which can be quantified
in terms of intensity, phase or intensity+phase of the OCT signal. The faster
the speed of the flowing RBCs, the greater is the flow signal; unless a
saturation level is reached.
In order to compute blood flow
measurements from the sequential B-scans, a number of algorithms are available.
These include:
1. Split-spectrum amplitude
decorrelation angiography (SSADA): This is a signal processing algorithm which
splits the OCT signal into different spectral bands to increase the number of
usable image frames without increasing the scanning time or decreasing scan
density. SSADA was able to produce angiograms of retinal and choroidal
vasculature with only 2 consecutive B-scans.
2. OCTA ratio analysis (OCTARA): This
is a motion contrast measure using a ratio method. The full spectrum is kept
intact and axial resolution preserved.
3. Optical microangiopathy (OMAG):
In this, calculations are based on the absolute difference between linear
intensities.
Certain other metrics used in
OCT-A are as follows:
1. Vessel density (VD): It is the
percentage area occupied by the large vessels and microvasculature over the
imaged area.
2. Flow index: A dimension-less
parameter between 0 and 1 representing the average decorrelation signal. It
measures the area of large vessels and the area and velocity of retinal
microvasculature.
3. Blood flow index: It is the mean flow
intensity in the vessel area normalized between 0 and 1 by dividing the full
dynamic range of blood flow signal intensity.
However, it should be remembered that
these indices are surrogate measures and their validity for measurement of
blood flow remains to be investigated.
OCT-A produces a 3D dataset of
scanned vascular tissue. Subsequently, automated or semi-automated segmentation
algorithms are used for accurate segmentation of the structural image in order
to have optimal evaluation of the retinal and choroidal vasculature. Appropriate
tissue layers or “slabs” can then be defined based on these reference planes.
The enface presentation of these
slabs produces angiograms similar to FA or ICG-A.
In Primary Angle Closure Glaucoma
(PACG) patients, immediately following an acute angle closure attack,
significantly decreased vessel densities in the peripapillary regions was
reported despite normal retinal nerve fiber layer thickness (RNFLT). The
peripapillary region refers to a 700µ wide elliptical annulus extending from
the optic disc boundary.
Comparison of PACG and Primary Open
Angle Glaucoma (POAG) eyes has shown the decrease in vessel density (VD) in
PACG to be more evenly distributed in the peripapillary region. Conversely, in
patients with POAG, there is lower perfusion in the infero-temporal
peripapillary region, corresponding to the frequent superonasal VF changes.
OCTA has the ability to visualize
and reliably quantify the optic nerve head (ONH) vasculature. A 25% decrease in
the flow index of ONH has been reported in glaucomatous eyes. This was found to
have a strong correlation with the pattern standard deviation in visual fields.
Patients with lamina cribrosa defects were also found to have lower vessel
density in the peripapillary region. Patients with uncontrolled IOP also have
significant reduction in ONH and peripapillary VD. Studies have also reported a
decrease in vessel density to be strongly associated with severity of VF
damage. The VD reduction in the optic disc was also found to be closely related
to ganglion cell complex thickness.
Artifacts with OCTA
1. Weak OCT signal= OCT signals
can be reduced globally due to media opacities, pupil vignetting and defocusing
of the light beam. OCT signal can also be lost below large caliber vessels or
hyper-reflective retinal lesions.
2. Motion artifacts= Bulk tissue
and saccadic eye movements can produce noise and motion artifacts. In order to overcome
these artifacts motion-correction-technology and eye-tracking have been used to
overcome motion artifacts. However, OCT-A can still show residual defects such
as motion lines, vessel duplication or vessel discontinuity. More advanced
processing algorithms are required to eliminate these artifacts from OCT-A.
3. Projection artifacts= When RBCs
flow in superficial vessels they cast time-varying shadows on the deeper
retinal layers. These flow projection artifacts lead to duplication of the
superficial vascular pattern on deeper microcirculation, as well as the
normally avascular outer retinal slab. OCT-A projection artifacts can lead to
inaccurate measurement of flow index and vessel density of deeper retinal
vasculature.
In order to overcome these
artifacts the superficial flow signal can be subtracted from the deeper en face angiograms, known as
“slab-subtraction” method. However, this process can disrupt the continuity of
vessels in the deeper vascular plexuses and potentially underestimate their
vessel density.
The newer “projection-resolved”
OCT-A suppresses the projected flow signal while preserving the natural
continuity of ocular microvasculature, allowing improved visualization and
quantification of different retinal vascular layers in normal and diseased
eyes.
Advantage of OCT-A
An advantage of OCT-A is that both
perfusion and corresponding structural information (en face OCT) of the different retinal layers are imaged and
measured respectively, on the same image. Thus, the combined analysis of the
images and measurements is useful in finding conformity between a structural
abnormality and its perfusion. The diagnostic accuracy of peripapillary and
whole-image angio-flow density for separation of glaucoma eyes from normal eyes
is similar to that of the RNFLT. The perfusion and peripapillary OCT-A sectors
show strong relationship with the sensitivity and defect values of the
spatially corresponding VF areas. Patients with uncontrolled IOP were found to
have significant reduction in ONH and peripapillary VD. Hollo has reported that
IOP reduction to atleast 50% of the pre-treatment value and below 18 mmHg
causes a significant increase in the peripapillary angioflow density.
Disadvantage of OCT-A
A disadvantage of OCT-A is the
small field of view, which restricts its image acquisition to the posterior
pole. It needs to be highlighted that lack of perfusion on OCTA does not
necessarily mean missing or obstructed vessels or lack of capillary perfusion;
in contrast, it simply means that at the time of image acquisition, no moving
RBCs were present in the location of the low perfusion or non-perfusion OCT-A
areas. OCT-A of the ONH is available with most machines; however, the presence
of large vessels and the variability and complexity of the 3D structure of the
disc makes it difficult to interpret the measurement results.