Retinal Nerve Fiber Layer Thickness (RNFLT) assessment
This is a primer regarding: "Retinal Nerve Fiber Layer Thickness (RNFLT) assessment using the CIRRUS Optical coherence tomography (OCT) machine".
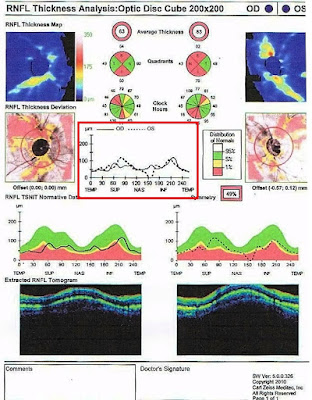
The Cirrus RNFL map represents a 6 x 6 mm cube of A-scan data centered
over the optic nerve in which a 3.4 mm diameter circle of RNFL data is
extracted to create what is referred to as the TSNIT map (temporal, superior,
nasal, inferior, temporal). It is displayed as a false color scale with
the thickness values referenced to a normative database. The TSNIT map displays
RNFL thickness values by quadrants and clock hours, and the RNFL peaks give a
sense of the anatomic distribution of nerve fiber axons represented by the
superior and inferior bundles that emanate from the optic nerve.
SD-OCT measurements are compared against an age-matched normative
database. The normative database for the Cirrus SD-OCT consisted of 284 healthy
individuals with an age range between 18 and 84 years (mean of 46.5 years).
Ethnically, 43% were Caucasian, 24% were Asians, 18% were African American, 12%
were Hispanic, 1% were Indian, and 6% were of mixed ethnicity. The refractive
error ranged from -12.00 D to +8.00 D. Due to this relatively small
normative database and wide variation of distribution of RNFL, many results
obtained by SD-OCT may be flagged as abnormal statistically in patients who are
not represented in the database and thus not necessarily representing real
disease. Clinicians should use caution to avoid overtreating “red disease” in these situations.
The Cirrus normative comparison for ONH parameters is based on the
patient’s age and disc size; while, for the RNFL is based on patient’s age. For
a particular age and disc size the patient is expected to have rim volume, C/D
ratio etc within certain ranges. Those parameters are shaded red, yellow, green
and white based on how they compare with normal ranges. When no normative data
is available for comparison, the parameters are shaded grey. This applies to
disc areas <1.3 mm2 or >2.5 mm2, since the database
has insufficient number of subjects with the disc areas of these sizes.
Average RNFL thickness indicates a patient's overall RNFL health. The
mean value for RNFL thickness in the general population is 92.9 +/- 9.4
microns. Typically, a normal, non-glaucomatous eye has an RNFL thickness of 80
microns or greater. An eye with an average RNFL thickness of 70 to 79 is
suspicious for glaucoma. An average thickness of 60 to 69 is seen in less than
5% of the normal population and implies glaucoma.
Based on a longitudinal study, the age-related rate of reduction in RNFL
thickness has been estimated to be -0.52 µm/year, -1.35 µm/year, and -1.25
µm/year for average, superior, and inferior RNFL respectively.
The best quality scans have signal strength greater than 8 (minimum
acceptable scan > 6).
(A). METHOD:
i.OCT images can be acquired through a 3mm pupil
in the absence of media opacities.
ii.However, a dilated pupil makes the procedure
easier and reduces acquisition errors.
iii. The patient can be asked to blink a few times
before image acquisition is started.
iv. A lubricant eyedrop can be instilled in case of
dry eyes.
v.The patient is asked to look into an internal
fixation target. (Green star-like in Cirrus)
vi.A circular or rarely a linear image is then
acquired.
(B). OCT REPORT PRINT-OUT: The Cirrus report shows assessment of the RNFL
and ONH of both eyes based on the 6mmx6mm cube captured by the Optic Disc Cube
200x200 scan. Some models of the OCT can display optic disc modules including
parameters such as rim area, disc area, average- and vertical- C/D ratio.
----------------------------------------------------------------------------------------------------------------------------------
1.
KEY
DATA: This forms the first part of information for the printout and
consists of the date and time of test; registration number, age, sex and date
of birth of the patient; technician, and the “signal strength”, which should be
above 8.
---------------------------------------------------------------------------------------------------------------------------------------------
2.
RNFLT
MAP: Topographic map of RNFL thickness in an hourglass shape of yellow
and red colors is typical of normal eyes. The color scale in microns on the
left of the image for reference is also provided. Warm colors (red, yellow)
represent thicker areas, while cooler colors (blue, green) represent thinner
areas.
---------------------------------------------------------------------------------------------------------------------------------
3.
RNFLT
DEVIATION MAP: It depicts the map of RNFL deviation from normal values
overlaid on an en face fundus image.
It also shows the machine-derived boundary of the cup and the disc and also the
calculation circle placement for the RNFL. It depicts the deviation from the
normative database in the form of color-coded superpixels, utilizing only
yellow and red colors. Green color is not used since most of the superpixels
would be green in a normal individual and would be present over most of the
image, obscuring the underlying fundus image. Thus, any region which is not red
or yellow indicates it is within normal limits. This map gives a gross clue
regarding the cup-disc ratio and position of the vessels in the cup. The RNFL
deviation map is useful to discuss the condition with the patient.
---------------------------------------------------------------------------------------------------------------------------------
4.
QUADRANT
AND CLOCK-HOUR RNFLT: A display of the average RNFLT along the whole
calculation circle is present on the top. Quadrant and clock hour averages are
given below and color coded in the same scales as rest of the report (based on
their P value with respect to deviation from age-matched data in the normative
database of the OCT machine). They specify the location of the pathology quadrant
and clock hour wise.
---------------------------------------------------------------------------------------------------------------------------------
5.
RNFL
NORMATIVE DATABASE: In the protocol, normative database is visualized
using a white-green-yellow-red color code. Color coding indicates the
particular position of the A-scan in the graph, the quadrant mean values and
the clock-position in the circular graphs and right and left columns of the
table of data. The patient’s RNFL is marked by a black (continuous [right eye] or
dashed line [left eye]). If the line dips into the red area, it indicates
thinning of the RNFL.
In an age-matched normal population, the percentiles regard each specific
measurement of RNFL in the following way:
(i) The thickest 5% of measurements fall in the
white area (White indicates >95%).
(ii)90% of measurements fall in the green area
(Green falls between 5% and <95%).
(iii)The thinnest 5% of measurements fall in or below
the yellow area (Yellow between 1% and <5%, indicating “suspect” area).
(iv)The thinnest 1% of measurements fall in
the red area. Measurements in red area are considered outside normal limits
(Red area falls in <1%).
---------------------------------------------------------------------------------------------------------------------------------
6.
SYMMETRY:
It indicates the extent of symmetry of the RNFLT in the TSNIT quadrants between
the 2 eyes.
---------------------------------------------------------------------------------------------------------------------------------
7.
RNFL-TSNIT
THICKNESS GRAPH: This shows the plot of RNFLT on the Y-axis (vertical)
and the retinal quadrants on the X-axis (horizontal). Normally, this has a
“double-hump” appearance due to the thicker RNFL in the superior and inferior
quadrants.
----------------------------------------------------------------------------------------------------------------------------------
8.
EXTRACTED
RNFL TOMOGRAMS: They display the reflectivity of the RNFL. They are not
of much clinical significance as far as decision making is considered.