GOOD CLINICAL PRACTICE
INTRODUCTION:
Good Clinical Practice (GCP) is a standard which needs to be
observed for the proper conduct of safe and quality research. It is an
“international, ethical and scientific quality standard for the design,
conduct, performance, monitoring, auditing, recording, analysis and reporting
of clinical trials involving the participation of human subjects”.
The term
“subject” is now regarded as politically-incorrect and demeaning so it is
suggested to use terms like “individuals” and “patients”. However, since the
GCP Guidelines still mention subject, I have retained the term wherever
necessary.
The basic principles of GCP
are provided in the ICH Harmonized Tripartite Guidelines [Guideline for Good Clinical
Practice E6(R1)]. The initial ICH-GCP Guideline was developed to provide a
unified standard for the European Union, Japan and United States to facilitate
the mutual acceptance of clinical data by the regulatory authorities in these
jurisdictions. However, later other countries came up with their own GCP
Guidelines based on the tripartite agreement.
These guidelines are necessary to follow during the conduct
of any clinical trial for 2 reasons:
1.
To assure the rights, safety, integrity,
confidentiality and well being of the human subjects during the trial.
2.
In order to generate credible data and to
maintain the integrity of data.
WHAT IS A CLINICAL TRIAL?
A clinical trial is any research study
that prospectively assigns human participants or groups of humans to one or
more health-related interventions to evaluate the effects on health outcomes.
It could be an investigation in human subjects, intended to
discover or verify the clinical, pharmacological and/or pharmacodynamic effects
of an investigational product (IP) and/or to identify any adverse reactions to
the IP and/or to study the absorption, distribution, metabolism and excretion
(ADME) of an IP with an objective of ascertaining it’s safety and/or efficacy.
NUREMBERG TRIAL AND THE DECLARATION OF HELSINKI:
The conduct of Clinical Trials (CT) should be based on
ethical principles derived from the
DECLARATION OF HELSINKI (DOH). During the
Nazi era unethical research was conducted on human beings which led to the
death of many individuals. The Japanese conducted similar research through
their Unit 731. In 1947, after the end of World War II, Nazi doctors and
scientists faced the
NUREMBERG TRIAL. As a result of the trial the
NUREMBERG CODE was developed which became the first codification of research guidelines
to protect human subjects. The Nuremberg Code set forth 10 Articles including
those relating to the assurance of safety of human beings and to assess the
scientific value of the research prior to the start of any experiment.
In 1964, the World Medical Association at its 18
th
General assembly in Helsinki extended the Nuremberg Code to include other
aspects of clinical research. The DOH has subsequently undergone further
revisions.
THE INTERNATIONAL CONFERENCE on HARMONIZATION (ICH)-GCP:
The ICH-GCP consists of the following elements:
1.
Glossary
2.
The principles of the ICH-GCP
3.
Institutional review Board (IRB) / Independent
Ethics Committee (IEC)
4.
Investigator
5.
Sponsor
6.
Clinical Trial Protocol and Protocol
Amendment(s)
7.
Investigator Brochure (IB)
8.
Essential Documents for the conduct of a
clinical trial
- 1.
The glossary explains terms such as: Adverse
Event (AE), Blinding/Masking, Case Report Form (CRF), monitoring, multicentre
Trial, Quality Assurance/Quality Control (QA/QC), randomization, Serious Adverse
Event (SAE), source data and others.
- 2.
There are 13 principles of GCP. These pertain
to, among others: ethical principles, rights of the subjects, scientific
soundness of the trial, involvement of IRB/IEC and investigators, freely given
informed consent, accurate reporting, confidentiality, good manufacturing
practice (GMP) of IP and assurance of quality in every aspect of the trial.
- 3.
The IRB/IEC is necessary to safeguard the
rights, safety and well-being of all trial subjects. Special attention should
be paid to vulnerable (not to be
unfairly targeted, e.g. pregnant women, children and prisoners) and underrepresented (not to be unfairly
excluded, e.g. minorities) groups. The IRB/IEC should obtain important
documents prior to start of the trial. An important document among these is the
written INFORMED CONSENT FORM(s)[ICF]. Informed consent is a “process” by which
a subject voluntarily confirms his/her willingness to participate in a CT,
after being made aware of all aspects of the trial that are relevant to the
subject’s decision to participate. Informed consent is documented by means of a
written, signed and dated ICF. In case the subject is not able to sign the ICF,
a LEGALLY AUTHORIZED REPRESENTATIVE (LAR) can sign the ICF.

- 4.
An investigator is a person who is qualified,
trained and experienced enough to assume responsibility for the proper conduct
of the trial. In order to make the investigator competent enough to handle the
trial, it is necessary to undergo the GCP training. The investigator (known as
the Principal Investigator or PI) may delegate some responsibilities to other
members of the study team by duly recording in the “DELEGATION LOG”. The
Sub-Investigator/s (SI) are those delegated by the PI for the conduct of the
study. The PI should be able to demonstrate adequate resources, provide medical
care to the trial subjects, communicate with the IRB/IEC, comply with the CT
protocol, be accountable for the IP at the site, randomize the procedures,
obtain informed consent, maintain records and reports, submit progress reports,
report on safety issues, inform the relevant persons, especially the subjects
in case of premature termination or suspension of the trial and to generate the
final report of the trial.
- 5.
A sponsor is an individual, company, institution
or organization which takes responsibility for the initiation, management
and/or financing of a trial. Sometimes, the sponsor may contract with a
Contract Research Organization (CRO) to perform one or more of the
duties/functions of the sponsor. The sponsor is responsible for QA/QC, trial
design and data management, selection of PI, compensation/financing of subjects
and study team, notification/submission to regulatory authorities, confirmation
of review by IRB/IEC, monitoring, audits and archiving of documents. Reporting
of AE/SAE is an important responsibility of the sponsor.
- 6.
A protocol is a document which describes how a
trial will be conducted (the objective/s, design, methodology, statistical
considerations and organization of a trial) and ensures the safety of the trial
subjects and integrity of the data collected.[Clinical Trial Protocol
development, accessible at https://hub.ucsf.edu/protocol-development
]. It provides general information regarding the trial, background information,
trial objectives and purpose, trial design, selection and withdrawal of
subjects, treatment of subjects, assessment of efficacy and safety, statistical
methods, ensure direct access to source data/documents for
monitoring/audit/IRB/IEC review, QA/QC, ethics, data handling and record
keeping, financing and insurance and publication policy.
- 7.
Investigator’s Brochure (IB) is a compilation of
the clinical and non-clinical data on the IP(s) which are relevant to the study
of the product(s) in human subjects. It provides the investigator with a clear
understanding of the possible risks and adverse reactions, specific tests,
observations and precautions required for a CT. It is based on available
physical, chemical, pharmaceutical, pharmacological, toxicological and clinical
information on the IP(s). It also guides the investigator to recognize and
treat possible overdose and Adverse Drug Reactions (ADR) based on previous
human experience and pharmacology of the IPs.
- 8.
Essential documents individually and
collectively permit evaluation of the conduct of a trial and the quality of the
data produced. They demonstrate the compliance of the investigator, sponsor and
monitor with the standards of GCP and applicable regulatory requirements. The
documents include those which are generated:
·
Prior to the commencement of the clinical phase
of the trial
·
During the conduct of the trial
·
After the completion/termination of the trial
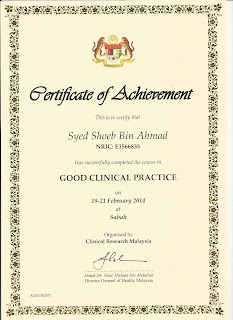
Further information regarding the GCP can be obtained online and
through various courses. It is imperative to obtain the GCP certificate
in order to conduct trials in an internationally acceptable manner.